Many people who find out they have cancer are able to survive the disease because of effective drugs.
Treating cancer with certain drugs is known as chemotherapy. The drugs contain powerful chemicals that kill cancer cells but also cause bad reactions in patients.
Although the drugs help keep patients alive, they cause extreme tiredness, stomach pain and the loss of hair. Some even result in mouth sores for patients. These problems are called side effects.
After many years of strong side effects, some patients and their doctors are talking to the U.S. Food and Drug Administration (FDA) about finding the lowest effective dose for cancer drugs.
In the past, drug companies tested to find the “maximum tolerable dose.” However, doctors and patients are asking drugmakers to think about a dose that will kill cancer cells with less severe side effects. Some patients might prefer the lower dose even if they need to use the drug longer.

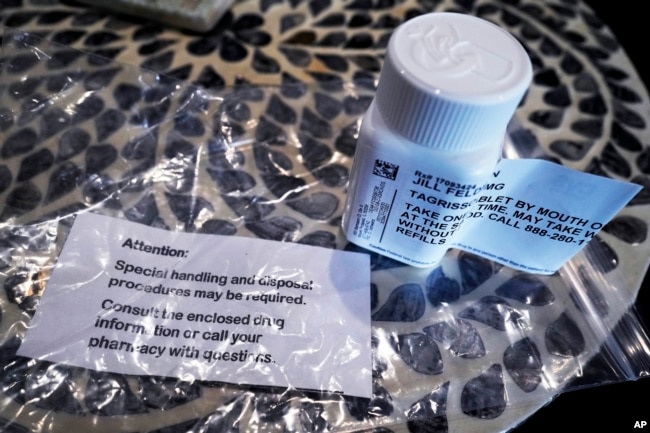
Jill Feldman of Illinois is 54. She has been treated for lung cancer for 15 years. She is happy to be alive – her parents died of lung cancer soon after they found out they had it. She said she is always in pain. She said her mouth always feels like it is burning.
With the help of her doctors, she receives a lower dose of her cancer drug. But she wants drug companies to research low doses when they are developing the treatments.
“No one should have to endure avoidable harmful effects of treatment,” she said.
Dr. Lillian Siu works on drug development at Princess Margaret Cancer Center in Toronto, Ontario. She said new cancer drugs are more precise than in the past. Some newer drugs target a mutation that causes cancer cell growth. Others cause the patient’s immune system to fight the cancer.
Siu says the question is whether patients can get “the same bang for their buck,” or useful result, with a lower dose of a drug. “You might only need a low dose to turn off that cancer driver,” she said.
An FDA spokesperson said there is a new program called Project Optimus that asks drugmakers to include patients who receive lower doses in their clinical trials.
Sometimes doctors lower doses during the later parts of testing. But other times, lower doses are called for only after the drug is approved and doctors try to reduce their patients’ side-effects.
Dr. Patricia LoRusso leads drug research at the Yale Cancer Center in Connecticut. She said the problem with using high doses is that patients start to feel bad, so they have to stop taking the drug. During that time, the cancer starts to come back.
In addition, some patients get results from a low dose, while others only get results from a high dose. That is called patient-to-patient variation. People’s liver and kidneys process cancer drugs differently which affects how much of the medicine reaches the cancer cells.
“The challenge is: Where is the sweet spot?” LoRusso said. A “sweet spot” means just the right amount.
One large group of patients has concerns about doses that are too high: women with breast cancer that has spread to other parts of their body. That kind of cancer is very difficult to treat. Without drugs, the cancer might spread even more. So many patients must be on cancer drugs for most of their lives. But they want to be able to enjoy their time, instead of feeling sick.
Dr. Julie Gralow is chief medical officer of the American Society of Clinical Oncology. She is working on a low-dose study of 500 patients who take two kinds of drugs for breast cancer.
She said the study will look at two kinds of treatments. One that starts patients on a low dose that increases if the patient does well. The other starts the patient at a high dose and then lowers if side effects are too difficult.

Lesley Kailani Glenn is a 58-year-old breast cancer patient from Oregon. She has been getting treatment for 11 years. She said she will need the drugs for the rest of her life.
“We want to try to live the best that we can, knowing that treatment is never-ever going to stop,” she said. Glenn has hiked California mountains and up high seaside hills in Italy while receiving treatment. She works with her doctor to change the amount of drug she receives based on her ability to tolerate it. She said the number one thing she dislikes is the feeling that she needs to use the bathroom all the time.
She does not want to lose her quality of life.
Project Optimus asks drugmakers to compare the results of different doses. It might sound like a good idea, but the drug companies have concerns. They say carrying out trials of separate doses slows down the development process.
Dr. Alice Shaw leads cancer drug development at Novartis, a Swiss drug company. She said the interest in lowering side effects by testing different doses needs to be weighed against getting a helpful new drug to cancer doctors.

She said it might be better to get the drugs on the market first.
But Dr. Timothy Yap of the MD Anderson Cancer Center in Houston, Texas said drug companies might not be seeing the problem correctly. He said they need to take the time early in the process to find the right dose. That way, more patients will be able to use their medicine.
“If the patients are not taking the drug, then it’s not going to work,” Yap said.
I’m Dan Friedell. And I’m Gena Bennett.
Dan Friedell adapted this story for Learning English based on a report by the Associated Press.
Quiz – Can ‘Less Be More’ with Cancer Drugs?

Start the Quiz to find out
________________________________________________
Words in This Story
sore –n. an area on the skin or tissue that is painful
dose –n. the right amount of medicine needed to get a good result
maximum –adj. the most
tolerable –adj. able to be suffered
endure –v. to live through something
precise –adj. very exact
mutation –n. a genetic change that, in the case of cancer, results in irregular cells
immune system –n. the system of cells and substances in the body that fight infection and sickness
clinical trial —n. tests that are done on real patients
